Items filtered by date: December 2020
What Do Plantar Warts Look Like?
Plantar warts are non-cancerous, rough growths that appear on pressure points located on the sole of the foot. They are caused by the human papillomavirus (HPV), which is spread through direct contact with a plantar wart or an object where HPV is present. Plantar warts are usually flat, and either brown, gray or flesh-colored. They can sometimes have black dots in the center, which are tiny capillaries that supply the wart with blood. Warts can grow individually or appear in clusters. They may be painful when you apply pressure to the bottom of the foot or walk on them. There are several types of therapies podiatrists can use to remove these warts permanently. If you notice a growth on the bottom of your foot that has the characteristics described here, please contact a podiatrist to confirm that what you see is a plantar wart and to receive proper care.
Plantar warts can be very uncomfortable. If you need your feet checked, contact one of our podiatrists from Toe-tal Family Footcare Associates. Our doctors will assist you with all of your foot and ankle needs.
About Plantar Warts
Plantar warts are the result of HPV, or human papillomavirus, getting into open wounds on the feet. They are mostly found on the heels or balls of the feet.
While plantar warts are generally harmless, those experiencing excessive pain or those suffering from diabetes or a compromised immune system require immediate medical care. Plantar warts are easily diagnosed, usually through scraping off a bit of rough skin or by getting a biopsy.
Symptoms
- Lesions on the bottom of your feet, usually rough and grainy
- Hard or thick callused spots
- Wart seeds, which are small clotted blood vessels that look like little black spots
- Pain, discomfort, or tenderness of your feet when walking or standing
Treatment
- Freezing
- Electric tool removal
- Laser Treatment
- Topical Creams (prescription only)
- Over-the-counter medications
To help prevent developing plantar warts, avoid walking barefoot over abrasive surfaces that can cause cuts or wounds for HPV to get into. Avoiding direct contact with other warts, as well as not picking or rubbing existing warts, can help prevent the further spread of plantar warts. However, if you think you have developed plantar warts, speak to your podiatrist. He or she can diagnose the warts on your feet and recommend the appropriate treatment options.
If you have any questions please feel free to contact our office located in Vista, CA and Las Vegas, NV . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
What Are Plantar Warts?
Plantar warts are described as small growths that appear on the heels or other areas of the feet that bear a large amount of weight. The pressure in these areas causes plantar warts to hide behind thick layers of skin called calluses. In most cases, plantar warts are not a serious health issue, and they usually go away without treatment. However, it is still important be mindful of them.
Plantar warts are caused by infections with human papillomavirus (HPV) in the outer layer of skin on the soles of the feet. The plantar warts then develop when the virus enters the body through weak spots at the bottom of the feet, such as tiny cuts and breaks. Plantar warts are not guaranteed for all who encounter the virus. Everyone responds differently to the affects of HPV.
Plantar warts are most common in the following groups: children and teenagers, people with weakened immune systems, people with history of plantar warts, and people who walk barefoot. Exposure to HPV is common in environments such as locker rooms or pool areas.
One of early signs to look out for is a callus, since many plantar warts hide behind them. You can also locate these warts by looking for small, fleshy, rough, grainy growths near the base of the toes and the heel. Early signs of plantar warts are shown by black pinpoints, which are small, clotted blood vessels. Lesions that interrupt normal lines and ridges in the skin of your foot may also be a sign of plantar warts. Any feeling of pain while walking or standing can also be a symptom of plantar warts.
Although most cases are not serious, some conditions may require a visit to your podiatrist. If you are uncertain that your lesion is a wart, if you have diabetes, or if you are experiencing bleeding, you may need to see a seek professional treatment. Your doctor may offer treatments such as prescribing stronger peeling medicine or using cryotherapy by applying liquid nitrogen to the wart. More serious cases may require minor surgery or laser treatment.
There are simple solutions available to help prevent plantar warts. One common task is to avoid walking barefoot in swimming pool areas and locker rooms, as this is where HPV is commonly present. Keeping your feet clean and dry, while changing shoes and socks daily can also help prevent future plantar warts. If you know someone who has plantar warts, it is important to avoid direct contact with their warts. You should also refrain from picking or scratching your wart if you happen to develop one.
Ways Seniors Can Maximize Foot Care
 As one ages, it becomes harder to reach down to the toes and keep toenails trimmed properly. In some cases, just gripping the clippers is difficult, if not impossible. At the same time, toenail growth decreases with age, resulting in thicker nails that are more difficult to trim. One way to soften the thicker nails and make them easier to cut is by soaking the feet for about 10 minutes in warm water. Thoroughly dry the feet, and use a clipper to make small cuts straight across the nail to lessen the chance of an ingrown toenail. If your toenails have both hardened and become discolored, you may also have developed a fungal infection. Such a condition can worsen rapidly and become painful. For that reason, it would be wise to contact a podiatrist immediately, as fungal infections may take months to eliminate. It is also suggested that seniors make regular appointments with a podiatrist for proper foot-care treatment as needed.
As one ages, it becomes harder to reach down to the toes and keep toenails trimmed properly. In some cases, just gripping the clippers is difficult, if not impossible. At the same time, toenail growth decreases with age, resulting in thicker nails that are more difficult to trim. One way to soften the thicker nails and make them easier to cut is by soaking the feet for about 10 minutes in warm water. Thoroughly dry the feet, and use a clipper to make small cuts straight across the nail to lessen the chance of an ingrown toenail. If your toenails have both hardened and become discolored, you may also have developed a fungal infection. Such a condition can worsen rapidly and become painful. For that reason, it would be wise to contact a podiatrist immediately, as fungal infections may take months to eliminate. It is also suggested that seniors make regular appointments with a podiatrist for proper foot-care treatment as needed.
Proper foot care is something many older adults forget to consider. If you have any concerns about your feet and ankles, contact one of our podiatrists from Toe-tal Family Footcare Associates. Our doctors can provide the care you need to keep you pain-free and on your feet.
The Elderly and Their Feet
As we age we start to notice many changes in our body, but the elder population may not notice them right away. Medical conditions may prevent the elderly to take notice of their foot health right away. Poor vision is a lead contributor to not taking action for the elderly.
Common Conditions
- Neuropathy – can reduce feeling in the feet and can hide many life-threatening medical conditions.
- Reduced flexibility – prevents the ability of proper toenail trimming, and foot cleaning. If left untreated, it may lead to further medical issues.
- Foot sores – amongst the older population can be serious before they are discovered. Some of the problematic conditions they may face are:
- Gouging toenails affecting nearby toe
- Shoes that don’t fit properly
- Pressure sores
- Loss of circulation in legs & feet
- Edema & swelling of feet and ankles
Susceptible Infections
Diabetes and poor circulation can cause general loss of sensitivity over the years, turning a simple cut into a serious issue.
If you have any questions please feel free to contact our office located in Vista, CA and Las Vegas, NV . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Elderly Foot Care
As you grow older, you will start to notice more problems with your feet due to wear and tear. This may also happen because the skin will start to become thin and lose elasticity. Some signs of aging feet are regular aches and pains, bunion development, and clawed toes.
Fortunately, there are ways you can improve comfort, relieve pain, and maintain mobility in your feet. One of the best ways to deal with aging feet is to exercise. If you keep active, your muscles will become toned which will then strengthen the arches in the foot and stimulate blood circulation.
It is important that you practice proper foot care to protect your aging feet. You should wash your feet in warm water on an everyday basis. Afterward, the feet need to be dried well and it is important to dry between the toes. Your toenails should be trimmed and kept under control; nails that are poorly cut may become ingrown. At the end of each day, performing an inspection of your feet will allow you to detect any ailments in their early stages.
As you grow older, it becomes more important that you wear comfortable shoes. Your shoes should be secure, and they should provide decent arch support. If you are looking to buy a new pair of shoes, it is best to look for a pair that are made from a breathable material. It is also helpful to have shoes that have a bit of extra room at the top of the shoe, especially if you suffer from swollen feet.
The most common foot problems that elderly people will encounter are bunions, calluses, corns, hammertoes, heel pain, and foot problems related to diabetes. Some other issues include arch pain, tarsal tunnel syndrome, Achilles tendonitis, and Morton’s neuroma
An annual foot examination is a great way for you to ensure that you do not have any serious health problems with your feet. You should talk to a podiatrist about the available treatment options for whichever foot issue you are dealing with.
What Causes Severe Pain Under the Big Toe?
Pain on the bottom of the foot just below the big toe is usually a sign of sesamoiditis, an inflammation of the two small bones under the first metatarsal. Repetitive weight-bearing activity (jumping or running, for instance), a change in footwear, or a gradually increased exercise regime are among the most common causes. You may feel a sharp pain to the affected area and react by cutting back or stopping the activity, getting different shoes, or possibly even limping. It can become very painful to walk on hard surfaces in bare feet. Causes include tissue injury, stress fractures of the sesamoid bones, or inflammation between the two small bones and the big toe (arthritis). High arches may be another culprit, causing more pressure under the ball of the foot. If you notice the pain growing more severe in this area of your foot, it is a good idea to make an appointment with a podiatrist who can determine the cause and offer appropriate treatment plans.
Sesamoiditis is an unpleasant foot condition characterized by pain in the balls of the feet. If you think you’re struggling with sesamoiditis, contact one of our podiatrists of Toe-tal Family Footcare Associates. Our doctors will treat your condition thoroughly and effectively.
Sesamoiditis
Sesamoiditis is a condition of the foot that affects the ball of the foot. It is more common in younger people than it is in older people. It can also occur with people who have begun a new exercise program, since their bodies are adjusting to the new physical regimen. Pain may also be caused by the inflammation of tendons surrounding the bones. It is important to seek treatment in its early stages because if you ignore the pain, this condition can lead to more serious problems such as severe irritation and bone fractures.
Causes of Sesamoiditis
- Sudden increase in activity
- Increase in physically strenuous movement without a proper warm up or build up
- Foot structure: those who have smaller, bonier feet or those with a high arch may be more susceptible
Treatment for sesamoiditis is non-invasive and simple. Doctors may recommend a strict rest period where the patient forgoes most physical activity. This will help give the patient time to heal their feet through limited activity. For serious cases, it is best to speak with your doctor to determine a treatment option that will help your specific needs.
If you have any questions please feel free to contact our office located in Vista, CA and Las Vegas, NV . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Sesamoiditis
Sesamoiditis is a condition that affects the joint that is just behind the big toe in the area known as the ball of the foot. It is most common in younger people and people who have just begun an exercise program. Since the sesamoid bones are like a pulley controlling the big toe, they can rub against each other and cause a gradual onset of pain. Pain may also be caused by the inflammation of tendons surrounding the bones. If ignored, sesamoiditis can lead to other, more serious problems such as severe irritation and fractures of the bones.
The cause of sesamoiditis is sudden increase in activity. The ball of your foot acts as a springboard to help you lift off when you are jogging or running. Sudden increase in the use of these bones or the tendon that controls them can cause irritation. The tendon then begins to develop inflammation and the joint begins to swell. People with smaller, bonier feet or those with a high arch are typically more susceptible to this condition.
Sesamoiditis is fairly simple to diagnose since the symptoms have a gradual onset rather than a sudden impact. The symptoms begin with slight irritation around the joint shortly after the increase in activity. The discomfort eventually turns to pain with light swelling and possibly redness. Although redness or bruising are rare, this may be a symptom. After each session of exercising, the aggravated joint becomes more irritated and increases into a very intense throbbing.
Treatment for sesamoiditis can vary depending on the severity of the situation. However, treatment is almost always approached in a noninvasive way. For a case that is just beginning the doctor may recommend a very strict rest period that will limit the activity allowed on the joint. If you must be active, a recommendation for as modified shoe or insole, along with bandaging and immobilizing the big toe will be made to ensure that pressure is not placed on the joint. For severe cases, it is typically recommended that the joint and the big toe be completely immobilized to allow adequate time to heal. Ice and an over the counter anti-inflammatory may can help with the pain and discomfort while you are at rest.
When you return to your regular exercise activities, it is recommended that you use an insole that will allow even distribution of impact to your entire foot, rather than just the balls of your foot. This will prevent further aggravation of the injury.
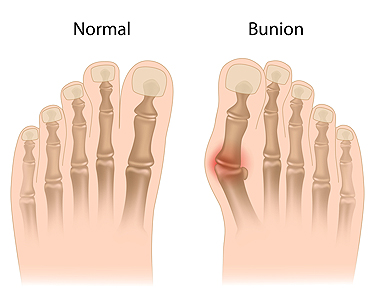
Are Bunions Genetic?
A bunion is a bony growth that occurs at the base of the big toe joint. Thought to be caused by faulty foot mechanics, bunions are often hereditary, meaning that they run in families. Wearing tight shoes with pointed toes can make bunions more likely to develop. Other than the deformity itself, symptoms of a bunion include pain, soreness, inflammation, redness, or a burning sensation around the bunion. It can become painful to wear certain shoes, walk, or stand for prolonged periods of time. Bunions progressively worsen without treatment, so it is strongly suggested that you see a podiatrist if you have a bunion that is bothering you.
If you are suffering from bunion pain, contact one of our podiatrists of Toe-tal Family Footcare Associates. Our doctors can provide the care you need to keep you pain-free and on your feet.
What Is a Bunion?
Bunions are painful bony bumps that usually develop on the inside of the foot at the joint of the big toe. As the deformity increases over time, it may become painful to walk and wear shoes. Women are more likely to exacerbate existing bunions since they often wear tight, narrow shoes that shift their toes together. Bunion pain can be relieved by wearing wider shoes with enough room for the toes.
Causes
- Genetics – some people inherit feet that are more prone to bunion development
- Inflammatory Conditions - rheumatoid arthritis and polio may cause bunion development
Symptoms
- Redness and inflammation
- Pain and tenderness
- Callus or corns on the bump
- Restricted motion in the big toe
In order to diagnose your bunion, your podiatrist may ask about your medical history, symptoms, and general health. Your doctor might also order an x-ray to take a closer look at your feet. Nonsurgical treatment options include orthotics, padding, icing, changes in footwear, and medication. If nonsurgical treatments don’t alleviate your bunion pain, surgery may be necessary.
If you have any questions, please feel free to contact our office located in Vista, CA and Las Vegas, NV . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Bunions
A bunion is an enlargement of the base joint of the toe that connects to the foot, often formed from a bony growth or a patch of swollen tissues. It is caused by the inward shifting of the bones in the big toe, toward the other toes of the foot. This shift can cause a serious amount of pain and discomfort. The area around the big toe can become inflamed, red, and painful.
Bunions are most commonly formed in people who are already genetically predisposed to them or other kinds of bone displacements. Existing bunions can be worsened by wearing improperly fitting shoes. Trying to cram your feet into high heels or running or walking in a way that causes too much stress on the feet can exacerbate bunion development. High heels not only push the big toe inward, but shift one's body weight and center of gravity towards the edge of the feet and toes, expediting bone displacement.
A podiatrist knowledgeable in foot structure and biomechanics will be able to quickly diagnose bunions. Bunions must be distinguished from gout or arthritic conditions, so blood tests may be necessary. The podiatrist may order a radiological exam to provide an image of the bone structure. If the x-ray demonstrates an enlargement of the joint near the base of the toe and a shifting toward the smaller toes, this is indicative of a bunion.
Wearing wider shoes can reduce pressure on the bunion and minimize pain, and high heeled shoes should be eliminated for a period of time. This may be enough to eliminate the pain associated with bunions; however, if pain persists, anti-inflammatory drugs may be prescribed. Severe pain may require an injection of steroids near the bunion. Orthotics for shoes may be prescribed which, by altering the pressure on the foot, can be helpful in reducing pain. These do not correct the problem; but by eliminating the pain, they can provide relief.
For cases that do not respond to these methods of treatment, surgery can be done to reposition the toe. A surgeon may do this by taking out a section of bone or by rearranging the ligaments and tendons in the toe to help keep it properly aligned. It may be necessary even after surgery to wear more comfortable shoes that avoid placing pressure on the toe, as the big toe may move back to its former orientation toward the smaller toes.
How Rheumatoid Arthritis Can Affect the Feet
In Rheumatoid Arthritis, the tissue lining within healthy joints is attacked by the body’s own immune system. This is very painful and can lead to joint damage and bone erosion. Rheumatoid Arthritis is a systemic disease, which can occur throughout the entire body. It often affects the feet, toes, and ankles, causing stiffness, pain, and abnormal warmth in joints and ligaments. A person’s quality of life can be affected by Rheumatoid Arthritis as well, since it can often reduce both mobility and the ability to participate in daily activities. When Rheumatoid Arthritis affects the feet, a podiatrist should be consulted to help relieve symptoms, decrease inflammation, and prevent joint damage. Possible treatments a podiatrist may use to treat Rheumatoid Arthritis include rest, medicine, orthotics, physical therapy, and steroid injections.
Arthritis can be a difficult condition to live with. If you are seeking treatment, contact one of our podiatrists from Toe-tal Family Footcare Associates. Our doctors can provide the care you need to keep you pain-free and on your feet.
Arthritic Foot Care
Arthritis is a term that is commonly used to describe joint pain. The condition itself can occur to anyone of any age, race, or gender, and there are over 100 types of it. Nevertheless, arthritis is more commonly found in women compared to men, and it is also more prevalent in those who are overweight. The causes of arthritis vary depending on which type of arthritis you have. Osteoarthritis for example, is often caused by injury, while rheumatoid arthritis is caused by a misdirected immune system.
Symptoms
- Swelling
- Pain
- Stiffness
- Decreased Range of Motion
Arthritic symptoms range in severity, and they may come and go. Some symptoms stay the same for several years but could potentially get worse with time. Severe cases of arthritis can prevent its sufferers from performing daily activities and make walking difficult.
Risk Factors
- Occupation – Occupations requiring repetitive knee movements have been linked to osteoarthritis
- Obesity – Excess weight can contribute to osteoarthritis development
- Infection – Microbial agents can infect the joints and trigger arthritis
- Joint Injuries – Damage to joints may lead to osteoarthritis
- Age – Risk increases with age
- Gender –Most types are more common in women
- Genetics – Arthritis can be hereditary
If you suspect your arthritis is affecting your feet, it is crucial that you see a podiatrist immediately. Your doctor will be able to address your specific case and help you decide which treatment method is best for you.
If you have any questions, please feel free to contact our office located in Vista, CA and Las Vegas, NV . We offer the newest diagnostic and treatment technologies for all your foot care needs.