Items filtered by date: December 2020
Peripheral Neuropathy and Its Impact on the Feet

Peripheral neuropathy is a condition characterized by damage to the nerves outside the brain and spinal cord. It often results in such symptoms as numbness, tingling, and weakness in the extremities. When it affects the feet, peripheral neuropathy can negatively impact mobility and quality of life. The nerves responsible for sensation and motor function in the feet may become impaired, leading to loss of sensation, burning pain, or hypersensitivity. These symptoms can make it challenging to walk or perform daily activities. Additionally, peripheral neuropathy can cause complications, such as foot ulcers and infections, particularly in individuals with diabetes. Regular foot care and monitoring are essential for preventing serious complications. Managing underlying conditions and adopting lifestyle changes, such as maintaining optimal blood sugar levels and wearing supportive footwear, can help alleviate symptoms and improve overall foot health for individuals with peripheral neuropathy. If you have this condition and your feet are affected, it is suggested that you are under the care of a podiatrist who can help you manage peripheral neuropathy.
Neuropathy
Neuropathy can be a potentially serious condition, especially if it is left undiagnosed. If you have any concerns that you may be experiencing nerve loss in your feet, consult with one of our podiatrists from Toe-tal Family Footcare Associates. Our doctors will assess your condition and provide you with quality foot and ankle treatment for neuropathy.
What Is Neuropathy?
Neuropathy is a condition that leads to damage to the nerves in the body. Peripheral neuropathy, or neuropathy that affects your peripheral nervous system, usually occurs in the feet. Neuropathy can be triggered by a number of different causes. Such causes include diabetes, infections, cancers, disorders, and toxic substances.
Symptoms of Neuropathy Include:
- Numbness
- Sensation loss
- Prickling and tingling sensations
- Throbbing, freezing, burning pains
- Muscle weakness
Those with diabetes are at serious risk due to being unable to feel an ulcer on their feet. Diabetics usually also suffer from poor blood circulation. This can lead to the wound not healing, infections occurring, and the limb may have to be amputated.
Treatment
To treat neuropathy in the foot, podiatrists will first diagnose the cause of the neuropathy. Figuring out the underlying cause of the neuropathy will allow the podiatrist to prescribe the best treatment, whether it be caused by diabetes, toxic substance exposure, infection, etc. If the nerve has not died, then it’s possible that sensation may be able to return to the foot.
Pain medication may be issued for pain. Electrical nerve stimulation can be used to stimulate nerves. If the neuropathy is caused from pressure on the nerves, then surgery may be necessary.
If you have any questions, please feel free to contact our office located in Vista, CA and Las Vegas, NV . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Neuropathy
Neuropathy is the weakness, numbness, and pain in the hands and feet due to damage to the peripheral nerves. The peripheral nerves are responsible for sending information from the brain and spinal cord to the rest of your body. Causes of Neuropathy include: traumatic injuries, infections, metabolic problems, exposure to toxins, and diabetes.
Diabetes is the most common cause, with more than half of the diabetic population developing some type of neuropathy. There are several types of neuropathy and they vary based on the damage of the nerves. Mononeuropathy is classified as only one nerve being damaged. When multiple nerves are affected, it is referred as polyneuropathy. One of the types of polyneuropathy is distal symmetric polyneuropathy. It is the most common for people with diabetes and starts when the nerves furthest away from the central nervous begin to malfunction. The symptoms begin with pain and numbness in the feet and then they travel up to the legs. A rarer form of polyneuropathy is acute symmetrical peripheral neuropathy, which is a severe type that affects nerves throughout the body and is highly associated with Guillain-Barre syndrome, an autoimmune disorder that attacks the peripheral nervous system and can be fatal. Although there are many types of neuropathy, most of them share the same symptoms such as pain, extreme sensitivity to touch, lack of coordination, muscle weakness, dizziness, and digestive problems. Since neuropathy affects the nerves, those affected should be careful of burns, infection and falling, as depleted sensations disguise such ailments.
The best way to prevent neuropathy is to manage any medical conditions such as diabetes, alcoholism, or rheumatoid arthritis. Creating and managing a healthy lifestyle can also go a long way. Having a healthy diet full of fruits, vegetables, whole grains and lean protein can keep the nerves healthy. These types of food have the nutrients to prevent neuropathy. Regularly exercising can help as well, but it is best to consult with a doctor about the right amount. In addition to diet and exercise, avoiding risk factors will also prevent neuropathy. This includes repetitive motions, cramped positions, exposure to toxic chemicals, smoking and overindulging on alcohol.
Understanding Common Causes of Foot Pain

Foot pain can affect individuals of all ages and lifestyles, impacting mobility and quality of life. One frequent reason for this type of pain is wearing improper footwear, such as shoes that are too tight, narrow, or lacking in support, leading to conditions like bunions, corns, and ingrown toenails. Overuse or repetitive strain on the feet, often seen in athletes or individuals with occupations that require prolonged standing or walking, can result in plantar fasciitis, stress fractures, and tendonitis. Additionally, structural abnormalities, such as flat feet, high arches, or misalignment of the bones, can contribute to chronic foot pain and discomfort. Systemic conditions like arthritis, diabetes, and circulatory disorders may also result in foot pain. Foot pain can be successfully treated by a podiatrist. If you have any type of foot pain, it is strongly suggested that you visit this type of doctor who can offer you appropriate treatment solutions.
Foot Pain
Foot pain can be extremely painful and debilitating. If you have a foot pain, consult with one of our podiatrists from Toe-tal Family Footcare Associates. Our doctors will assess your condition and provide you with quality foot and ankle treatment.
Causes
Foot pain is a very broad condition that could be caused by one or more ailments. The most common include:
- Bunions
- Hammertoes
- Plantar Fasciitis
- Bone Spurs
- Corns
- Tarsal Tunnel Syndrome
- Ingrown Toenails
- Arthritis (such as Gout, Rheumatoid, and Osteoarthritis)
- Flat Feet
- Injury (from stress fractures, broken toe, foot, ankle, Achilles tendon ruptures, and sprains)
- And more
Diagnosis
To figure out the cause of foot pain, podiatrists utilize several different methods. This can range from simple visual inspections and sensation tests to X-rays and MRI scans. Prior medical history, family medical history, and any recent physical traumatic events will all be taken into consideration for a proper diagnosis.
Treatment
Treatment depends upon the cause of the foot pain. Whether it is resting, staying off the foot, or having surgery; podiatrists have a number of treatment options available for foot pain.
If you have any questions, please feel free to contact our office located in Vista, CA and Las Vegas, NV . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Foot Pain
Our feet are arguably the most important parts of our bodies because they are responsible for getting us from place to place. However, we often don’t think about our feet until they begin to hurt. If you have pain in your feet, you need to first determine where on the foot you are experiencing it to get to the root of the problem. The most common areas to feel pain on the foot are the heel and the ankle.
Heel pain is most commonly attributed to a condition called plantar fasciitis. Plantar fasciitis occurs when the plantar fascia, which is the band of tough tissue connecting the heel bone to the toes becomes inflamed. Plantar fasciitis pain is usually worse in the morning, and it tends to go away throughout the day. If you have plantar fasciitis, you should rest your foot and do heel and foot muscles stretches. Wearing shoes with proper arch support and a cushioned sole has also been proven to be beneficial.
Some common symptoms of foot pain are redness, swelling, and stiffness. Foot pain can be dull or sharp depending on its underlying cause. Toe pain can also occur, and it is usually caused by gout, bunions, hammertoes, ingrown toenails, sprains, fractures, and corns.
If you have severe pain in your feet, you should immediately seek assistance from your podiatrist for treatment. Depending on the cause of your pain, your podiatrist may give you a variety of treatment options.
Where Are Plantar Warts Found?

Plantar warts, medically termed Verruca plantaris, are common skin growths caused by the human papillomavirus, or HPV. These warts typically appear on the soles of the feet, often in areas subjected to pressure or friction, such as the heels or balls of the feet. Plantar warts often manifest as small, rough, grainy lesions with black dots, or wart seeds, scattered throughout. These black dots are actually tiny blood vessels. While plantar warts are usually harmless, they can cause discomfort or pain, especially when walking or standing. The HPV virus enters the body through small cuts or breaks in the skin, making individuals who frequently walk barefoot in communal areas more susceptible to infection. Treatment options for plantar warts range from remedies like salicylic acid patches or freezing kits to medical procedures performed by podiatrists. Seeking prompt treatment is essential to alleviate symptoms and prevent the spread of plantar warts to other areas of the feet or other individuals. If you have a plantar wart, it is suggested that you schedule an appointment with a podiatrist who can offer the best treatment option for you.
Plantar warts can be very uncomfortable. If you need your feet checked, contact one of our podiatrists from Toe-tal Family Footcare Associates. Our doctors will assist you with all of your foot and ankle needs.
About Plantar Warts
Plantar warts are the result of HPV, or human papillomavirus, getting into open wounds on the feet. They are mostly found on the heels or balls of the feet.
While plantar warts are generally harmless, those experiencing excessive pain or those suffering from diabetes or a compromised immune system require immediate medical care. Plantar warts are easily diagnosed, usually through scraping off a bit of rough skin or by getting a biopsy.
Symptoms
- Lesions on the bottom of your feet, usually rough and grainy
- Hard or thick callused spots
- Wart seeds, which are small clotted blood vessels that look like little black spots
- Pain, discomfort, or tenderness of your feet when walking or standing
Treatment
- Freezing
- Electric tool removal
- Laser Treatment
- Topical Creams (prescription only)
- Over-the-counter medications
To help prevent developing plantar warts, avoid walking barefoot over abrasive surfaces that can cause cuts or wounds for HPV to get into. Avoiding direct contact with other warts, as well as not picking or rubbing existing warts, can help prevent the further spread of plantar warts. However, if you think you have developed plantar warts, speak to your podiatrist. He or she can diagnose the warts on your feet and recommend the appropriate treatment options.
If you have any questions please feel free to contact our office located in Vista, CA and Las Vegas, NV . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
What Are Plantar Warts?
Plantar warts are described as small growths that appear on the heels or other areas of the feet that bear a large amount of weight. The pressure in these areas causes plantar warts to hide behind thick layers of skin called calluses. In most cases, plantar warts are not a serious health issue, and they usually go away without treatment. However, it is still important be mindful of them.
Plantar warts are caused by infections with human papillomavirus (HPV) in the outer layer of skin on the soles of the feet. The plantar warts then develop when the virus enters the body through weak spots at the bottom of the feet, such as tiny cuts and breaks. Plantar warts are not guaranteed for all who encounter the virus. Everyone responds differently to the affects of HPV.
Plantar warts are most common in the following groups: children and teenagers, people with weakened immune systems, people with history of plantar warts, and people who walk barefoot. Exposure to HPV is common in environments such as locker rooms or pool areas.
One of early signs to look out for is a callus, since many plantar warts hide behind them. You can also locate these warts by looking for small, fleshy, rough, grainy growths near the base of the toes and the heel. Early signs of plantar warts are shown by black pinpoints, which are small, clotted blood vessels. Lesions that interrupt normal lines and ridges in the skin of your foot may also be a sign of plantar warts. Any feeling of pain while walking or standing can also be a symptom of plantar warts.
Although most cases are not serious, some conditions may require a visit to your podiatrist. If you are uncertain that your lesion is a wart, if you have diabetes, or if you are experiencing bleeding, you may need to see a seek professional treatment. Your doctor may offer treatments such as prescribing stronger peeling medicine or using cryotherapy by applying liquid nitrogen to the wart. More serious cases may require minor surgery or laser treatment.
There are simple solutions available to help prevent plantar warts. One common task is to avoid walking barefoot in swimming pool areas and locker rooms, as this is where HPV is commonly present. Keeping your feet clean and dry, while changing shoes and socks daily can also help prevent future plantar warts. If you know someone who has plantar warts, it is important to avoid direct contact with their warts. You should also refrain from picking or scratching your wart if you happen to develop one.
Definition and Location of Heel Spurs
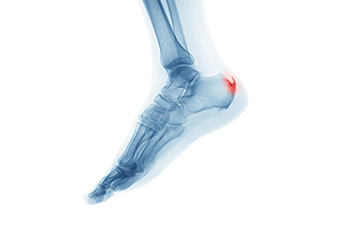
Heel spurs, a common foot condition, refer to calcium deposits that develop on the underside of the heel bone. They often form in response to repetitive stress or strain on the foot's ligaments and muscles. While heel spurs themselves may not cause pain, they can contribute to discomfort and inflammation in the surrounding tissues, leading to conditions such as plantar fasciitis or Achilles tendonitis. Heel spurs typically occur in the area where the plantar fascia, a thick band of tissue that runs along the bottom of the foot, attaches to the heel bone. As the body attempts to heal and repair the damaged tissues, calcium deposits may accumulate over time, resulting in the formation of a bony protrusion. Understanding the location and nature of heel spurs is essential for effective treatment and management strategies. If you have heel pain, it is strongly suggested that you consult a podiatrist who can accurately diagnose heel spurs and offer you appropriate treatment methods.
Heel spurs can be incredibly painful and sometimes may make you unable to participate in physical activities. To get medical care for your heel spurs, contact one of our podiatrists from Toe-tal Family Footcare Associates. Our doctors will do everything possible to treat your condition.
Heels Spurs
Heel spurs are formed by calcium deposits on the back of the foot where the heel is. This can also be caused by small fragments of bone breaking off one section of the foot, attaching onto the back of the foot. Heel spurs can also be bone growth on the back of the foot and may grow in the direction of the arch of the foot.
Older individuals usually suffer from heel spurs and pain sometimes intensifies with age. One of the main condition's spurs are related to is plantar fasciitis.
Pain
The pain associated with spurs is often because of weight placed on the feet. When someone is walking, their entire weight is concentrated on the feet. Bone spurs then have the tendency to affect other bones and tissues around the foot. As the pain continues, the feet will become tender and sensitive over time.
Treatments
There are many ways to treat heel spurs. If one is suffering from heel spurs in conjunction with pain, there are several methods for healing. Medication, surgery, and herbal care are some options.
If you have any questions feel free to contact our office located in Vista, CA and Las Vegas, NV . We offer the latest in diagnostic and treatment technology to meet your needs.
Heel Spurs
Heel spurs are the result of calcium deposits that cause bony protrusions on the underside of the heel. Heel spurs are usually painless, but they have the potential to cause heel pain. Heel spurs tend to be associated with plantar fasciitis, which is a condition that causes inflammation of the band of connective tissue that runs along the bottom of the foot. They most often occur to athletes whose sports involve a lot of running and jumping.
Some risk factors for developing heel spurs include running and jogging on hard surfaces, being obese, wearing poorly fitting shoes, or having walking gait abnormalities.
It is possible to have a heel spur without showing signs of any symptoms. However, if inflammation develops at the point of the spur’s formation, you may have pain while walking or running. In terms of diagnosis, sometimes all a doctor needs to know is that the patient is experiencing a sharp pain localized to the heel to diagnose a heel spur. Other times, an x-ray may be needed to confirm the presence of a heel spur.
Heel spurs can be prevented by wearing well-fitting shoes that have shock-absorbent soles. You should also be sure that you are choosing the right shoe for the activity you want to partake in; for example, do not wear walking shoes when you want to go on a run. Additionally, maintaining a healthy weight can be beneficial toward preventing heel spurs, as it will prevent an excess amount of pressure being placed on the ligaments.
There are a variety of treatment options for people with heel spurs. Some of these include stretching exercises, physical therapy, shoe inserts, or taping and strapping to rest stressed muscles and tendons. If you have heel pain that lasts longer than a month, don’t hesitate to seek help from a podiatrist. Your doctor can help you determine which treatment option is best for you.
Symptoms of Rheumatoid Arthritis in Feet

Rheumatoid arthritis, abbreviated RA, is a chronic autoimmune disorder that primarily targets the joints, often causing inflammation, pain, and stiffness. When it comes to the feet, RA can manifest in various ways, affecting both the joints and surrounding tissues. A common symptom is morning stiffness, where the feet feel tender and stiff upon waking or after periods of inactivity. Swelling, redness, and warmth around the joints, particularly in the toes and ankles, are common indicators of inflammation associated with RA. As the disease progresses, deformities such as bunions or hammertoes may develop, altering the alignment and structure of the feet. Additionally, RA can lead to persistent pain and discomfort during movement, impacting mobility and overall function. If you are experiencing symptoms of RA in your feet, it is suggested that you are under the care of a podiatrist who can help you manage this condition.
Because RA affects more than just your joints, including the joints in your feet and ankles, it is important to seek early diagnosis from your podiatrist if you feel like the pain in your feet might be caused by RA. For more information, contact one of our podiatrists of Toe-tal Family Footcare Associates. Our doctors will assist you with all of your podiatric concerns.
What Is Rheumatoid Arthritis?
Rheumatoid Arthritis (RA) is an autoimmune disorder in which the body’s own immune system attacks the membranes surrounding the joints. Inflammation of the lining and eventually the destruction of the joint’s cartilage and bone occur, causing severe pain and immobility.
Rheumatoid Arthritis of the Feet
Although RA usually attacks multiple bones and joints throughout the entire body, almost 90 percent of cases result in pain in the foot or ankle area.
Symptoms
- Swelling and pain in the feet
- Stiffness in the feet
- Pain on the ball or sole of feet
- Joint shift and deformation
Diagnosis
Quick diagnosis of RA in the feet is important so that the podiatrist can treat the area effectively. Your doctor will ask you about your medical history, occupation, and lifestyle to determine the origin of the condition. Rheumatoid Factor tests help to determine if someone is affected by the disease.
If you have any questions please feel free to contact our office located in Vista, CA and Las Vegas, NV . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
